By Brooke Siefker, Emergency Management Specialist
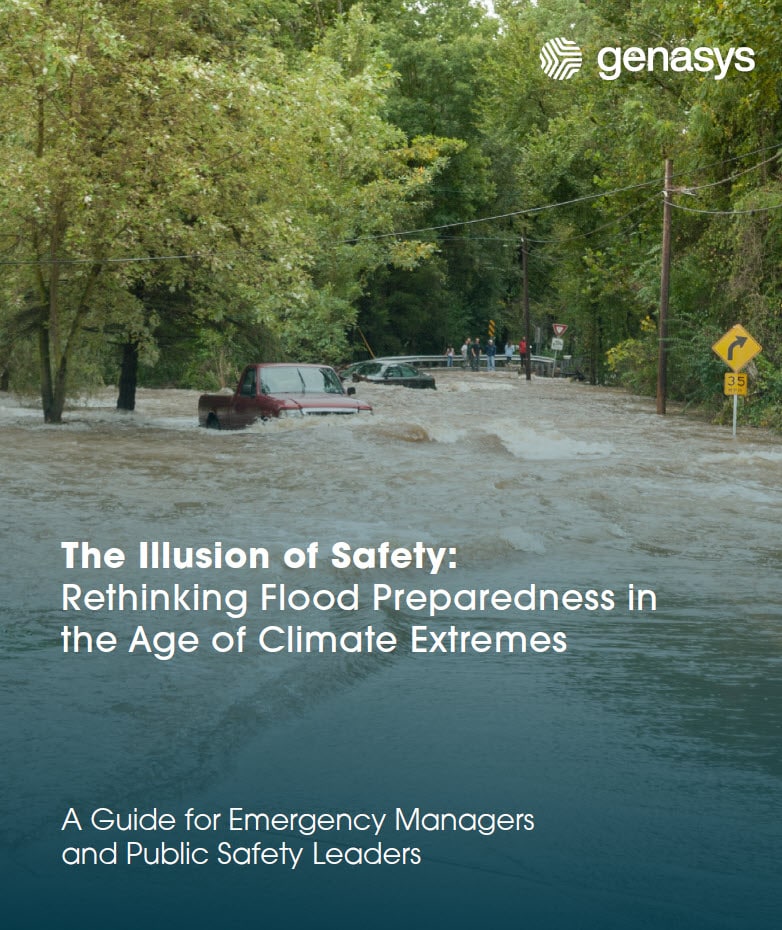
When disaster strikes—whether it’s a fast-moving wildfire or a devastating flood—the ability to maintain healthcare services becomes a matter of life and death.
Natural disasters not only disrupt daily life but can overwhelm healthcare systems, leaving vulnerable populations at risk. Emergency rooms face surges of patients, medical supply chains are disrupted, and access to life-saving treatments, like dialysis or chemotherapy, may be interrupted.
Maintaining communications is critical to ensure that communities can weather the disaster and aftermath and continue to receive essential care when it’s needed most.
Providing Healthcare Before, During, and After a Major Disaster
Healthcare continuity during disasters hinges on robust preparedness, innovative technology, and seamless communication between providers, patients, and emergency responders. From implementing real-time alert systems to creating emergency action plans tailored to specific disaster scenarios, healthcare systems must take proactive steps to remain operational.
From immediate disaster medicine needs to long-term continuity for chronic conditions like dialysis and chemotherapy, healthcare providers and first responders will see and treat patients in a variety of situations, including:
- Initial Emergency Medical Care
- Treat injuries like burns and smoke inhalation, fractures, lacerations, or trauma caused by the disaster.
- Manage acute issues from smoke inhalation (during wildfires), or drowning, electrocution, or hypothermia (during hurricanes and floods).
- Manage mental health related issues like anxiety, PTSD, and acute stress reactions.
- Evacuation Support
- Transport compromised patients from high-risk areas to safe zones.
- Ensure the immediate continuity of care for hospitalized patients, those in nursing homes, or the homebound on oxygen or ventilators.
- Shelter Health Services
- Set up medical stations in evacuation shelters to address acute and chronic health needs.
- Provide mental health support and crisis counseling.
- Public Health Monitoring
- Assess the risk of disease outbreaks, such as cholera or leptospirosis in floods, or respiratory illnesses in wildfires.
- Ensure a clean water supply and sanitation to prevent the spread of infections.
- Chronic Disease Management
- Ensure access to medications and medical devices (e.g., insulin for diabetics, oxygen for those with COPD, and dialysis for end-stage renal failure).
- Provide care for dialysis patients or those undergoing cancer treatment.
- Rehabilitation Services:
- Address long-term health impacts of the disaster, such as physical rehabilitation or ongoing mental health support.
Key Healthcare Issues and Challenges
Disasters place immense pressure on healthcare systems and first responders, as they must navigate a surge in demand while working in hazardous and unpredictable conditions. Emergency rooms often become overcrowded, and healthcare professionals are tasked with triaging a wide range of injuries, from minor cuts to life-threatening conditions like burns, respiratory distress, or cardiac events.
Vulnerable populations, such as the elderly, children, individuals with chronic illnesses, and those with disabilities, require specialized attention, adding complexity to already strained operations. Additionally, disruptions to supply chains can lead to shortages of critical medications, medical supplies, and equipment, further complicating the ability to provide effective care.
The aftermath of a disaster brings its own set of challenges for first responders and healthcare professionals, as the focus shifts to addressing long-term health impacts and preventing the spread of communicable diseases. Contaminated water, inadequate sanitation, and crowded living conditions in shelters create fertile ground for outbreaks of diseases such as cholera, hepatitis, or respiratory infections. Mental health issues, including PTSD and anxiety, often surge among both disaster victims and first responders, requiring additional resources and support.
These challenges underscore the need for comprehensive disaster preparedness and recovery plans to mitigate the impact on public health which includes the ability to communicate with response teams before, during and after a disaster event. Challenges include:
- Increased Demand for Services
- Overwhelmed healthcare systems and facilities, leading to delays in care.
- Shortages of medical supplies, medications, and personnel.
- Vulnerable Populations
- Higher risk for the elderly, children, pregnant women, and individuals with disabilities.
- Challenges in evacuating and caring for these groups.
- Mental Health Challenges
- Increased stress, anxiety, and PTSD among disaster survivors and responders.
- Grief counseling and trauma recovery for those who lost homes or loved ones.
- Communicable Disease and Environmental Health Risks
- Spread of diseases due to overcrowding in shelters and compromised hygiene.
- Vector-borne diseases (e.g., diseases caused by mosquitoes, parasites, bacteria).
- Exposure to hazardous materials (e.g., toxic ash in wildfires or contaminated floodwater).
- Access to Care Barriers
- Disruption of transportation and communication networks.
- Closure or damage to healthcare facilities.
Preparedness and Solutions
Effective disaster preparedness is key when mitigating the impact on healthcare systems and ensuring communities receive the support, they need during emergencies. A well-developed disaster response plan is essential, outlining protocols for triage, patient evacuation, and resource allocation. These plans should be practiced regularly to identify and address potential gaps.
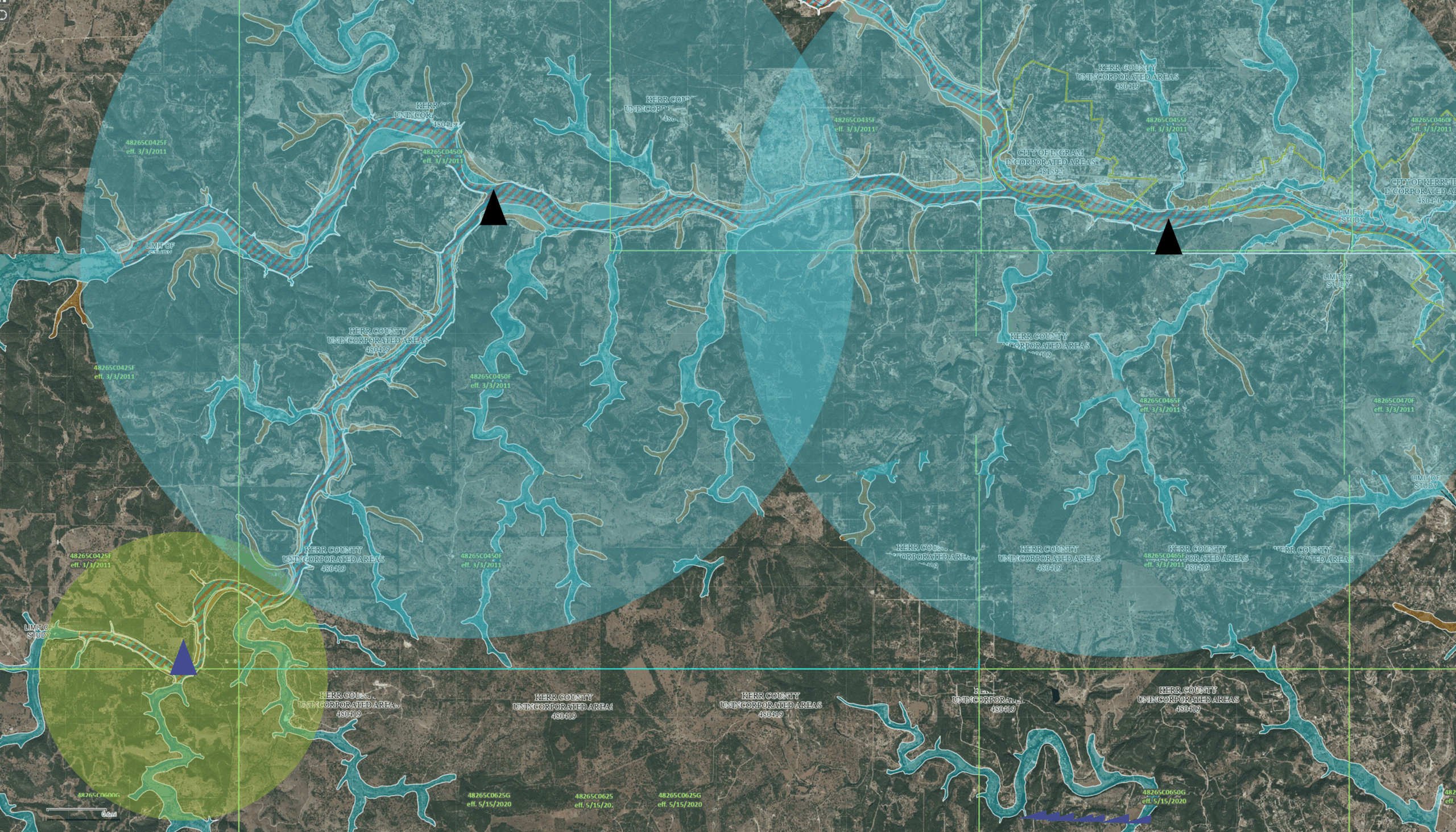
Technology exists today that allows first responders and emergency healthcare teams to communicate via evacuation software and secure, compliant messaging apps that place a high priority on collaborative support and real-time awareness during the most complex of situations. This is especially important in today’s fast-moving disasters where entire communities can be decimated in a matter of hours.
Deploying mobile clinics in the initial phases of an emergency is another innovative solution that brings critical care directly to affected areas when traditional healthcare facilities are inaccessible. These clinics can provide first aid, distribute medications, and deliver care to vulnerable populations who may otherwise be left behind.
Building supply resilience is critical for maintaining care during a crisis. Stockpiling essential medications, portable medical equipment, and backup power supplies ensure continuity even when supply chains are disrupted.
A Final Thought on Communication and Collaboration
Collaboration between healthcare organizations, emergency responders, and government agencies strengthens overall disaster response capabilities. Robust communication systems are vital, enabling seamless coordination between first responders, hospitals, and community leaders. By integrating these solutions into disaster preparedness efforts, healthcare systems can better safeguard lives and ensure a more effective response.
Contact Genasys to learn more about EVAC evacuation software and CONNECT cross-agency messaging software.